Publications Update # 103

Non-Medical Article of the Week
For the fellows graduating and joining new practices - Don’t hand your purpose to the new employer or their marketing team—own it. Find the path that fits you niche: competence (outstanding clinical care), culture (how you work together), or cause (a social mission). Pick what rings true, put it in writing, then prove it—perform, and lead in ways that back it up. Many practices thrive by doubling down on clinical excellence or a strong culture; you don’t need a grand crusade unless it’s genuine. Purpose only matters when you—and your team—model it in every consult, hand-off, and decision. This HBR article is a great read.
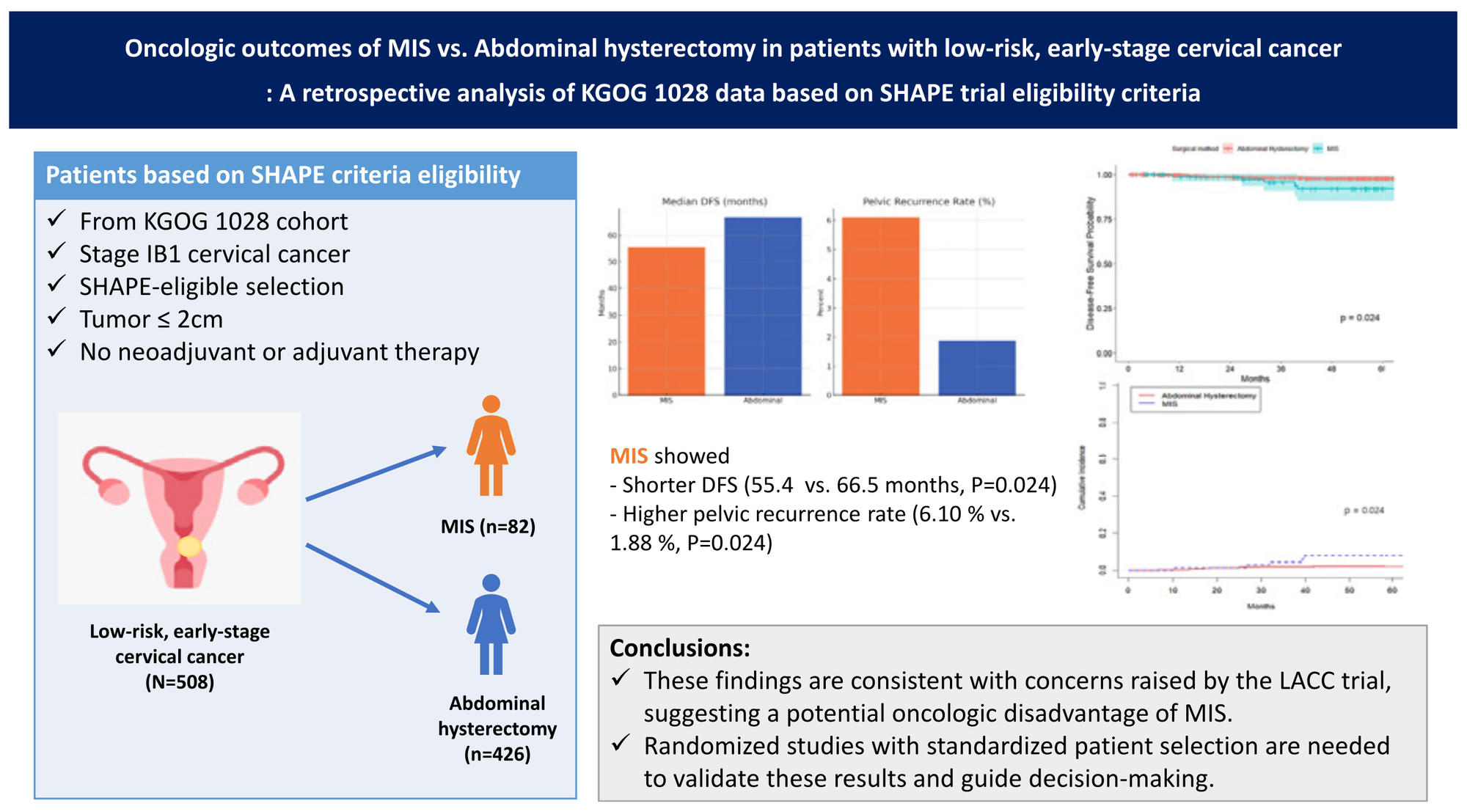
Cervical Cancer
In the seven-plus years since the LACC trial, I have yet to meet a single patient willing to accept a higher risk of recurrence just to have her radical hysterectomy done minimally invasively. For most of us, that debate was over—pending the ROCC and RACC trials, which might resurrect a very different, rigorously vetted MIS radical hysterectomy if they can prove true non-inferiority to the open approach.
Then came the SHAPE trial, and it muddied the waters. Remember: 83% of cases in the simple-hysterectomy arm and 71% in the radical-hysterectomy arm were performed minimally invasively (MIS). The investigators themselves warned us not to over-extrapolate and stay away from “MIS is safe for simple hysterectomy in cervical cancer” narrative as the trial was not powered to detect this difference. After getting burned by unvalidated MIS in this disease once already, that caution felt warranted.
Fast-forward to today’s featured paper: KGOG compared MIS with open simple hysterectomy in patients who fit SHAPE criteria. The disease-free survival 55 months vs 66.5 months, and pelvic recurrences 6% vs 2% (both p < 0.05) in favor of open surgery once again reemphasize the fact that MIS (without the cautions built in ROCC and RACC trials) in cervical cancer is definitely NOT safe.
T.L;D.R: Until we see solid evidence to the contrary, I’m sticking with—and strongly recommending—open simple hysterectomy for cervical-cancer patients meeting SHAPE criteria for simple hysterectomy, especially those with residual cervical disease.
Related Content on GYOEDU
Read about how to reduce the risk of recurrence in cervical cancer patients undergoing radical hysterectomy by first performing conization before surgery (from Publications Update # 99)
Endometrial Cancer
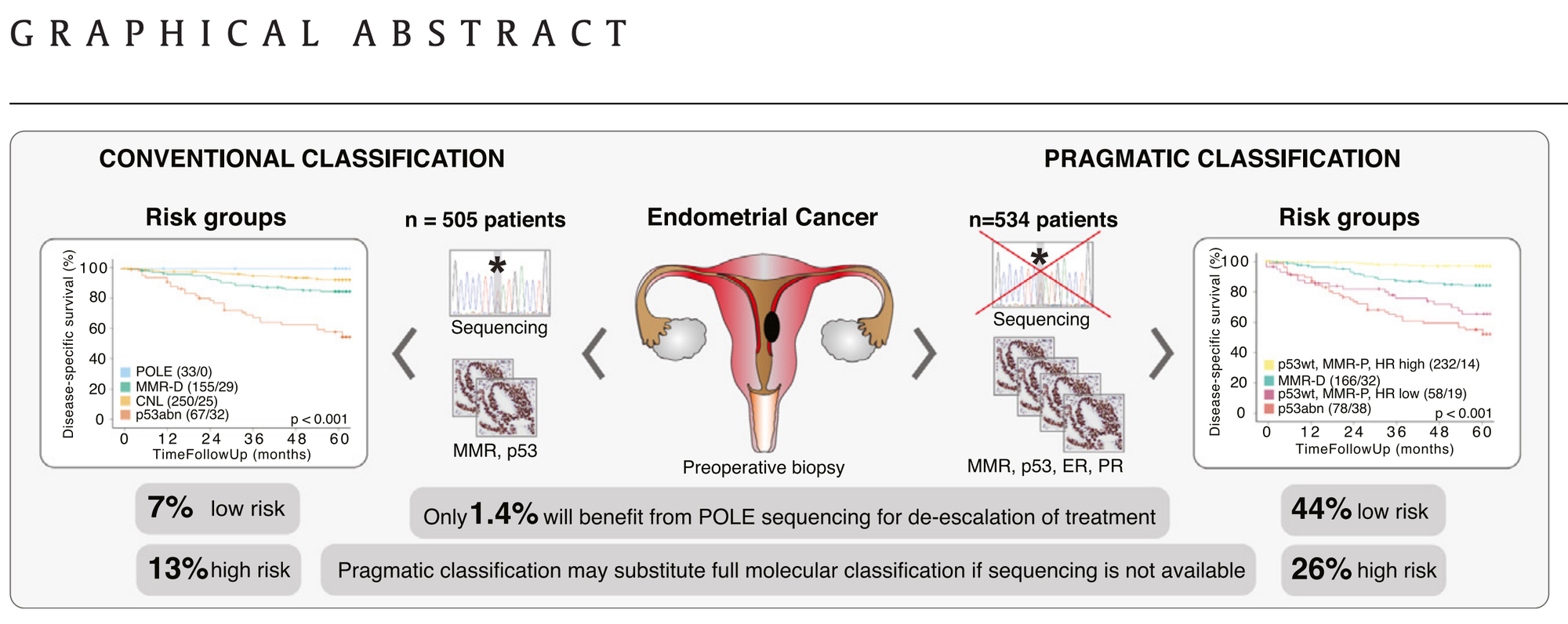
Pragmatic molecular classification has the potential to replace expensive genomic sequencing with four pre-operative immunohistochemistry stains (MMR, p53, ER, PR). In this paper, Berg et al. demonstrated that their IHC algorithm stratifies endometrial cancers into MMR-d, p53-abn, HR-low, and HR-high groups, achieving prognostic separation equivalent to the TCGA/ProMisE model, while eliminating routine POLE testing and delivering results before surgery based on endometrial biopsies.
How to think about this paper?
Here is how these groups map onto each other. Primarily, the POLE group overlaps heavily with the MMR-p, p53wt, and hormone receptor-high group.
| POLE | MMR-D | CNL | p53abn | Total | |
|---|---|---|---|---|---|
| Conventional % | 7 | 31 | 50 | 13 | 100 |
| Maps to | ↘︎ HR-high ≈ 6 ↘︎ HR-low ≈ 1 |
↘︎ MMR-D 31 | ↘︎ HR-high 43 ↘︎ HR-low 11 |
↘︎ p53abn 13 |
Previously, I sent a different paper in the Publications Update # 86 with a very similar idea of pragmatic molecular testing in endometrial cancer. The difference in this paper is that the authors used ER receptor only instead of a combination of ER/PR.
Enjoying the GYOEDU Newsletters?
A video explaining the Less is More approach was previously sent in Publications Update # 86. Watch a video explaining the paper
Video will only work on the website.
A similar breakdown of the categories for Perrone et al
| POLE-mut | MMR-deficient (MMR-d) | NSMP (no specific molecular profile) |
p53-abnormal (p53abn) | Total | |
|---|---|---|---|---|---|
| Conventional % | 6 | 25 | 47 | 21 | 100 |
| Maps to IHC-only model % | ↘︎ MMRp-ERpos ≈ 5 | ↘︎ MMRd 25 | ↘︎ MMRp-ERpos ≈ 38 ↘︎ MMRp-ERneg ≈ 9 |
↘︎ p53abn 21 |
In other words, POLE mut can be infered by the hormone receptor status to a very high degree based on these two papers. Patients with best prognosis are MMR-p, p53-wt, high-hormone receptor
Question(s) from the Question Bank
Question 1
A 70-year-old woman with a history of persistent cough and active smoking is scheduled for an open exploratory laparotomy and debulking for suspected advanced ovarian cancer. Preoperative pulmonary function tests are obtained. Which single preoperative pulmonary function test parameter is MOST predictive of an increased risk for major postoperative pulmonary complications (e.g., pneumonia, respiratory failure) in this patient?
A. Forced Vital Capacity (FVC) less than 70% predicted.
B. Forced Expiratory Volume in 1 second (FEV1) less than 1.0-1.5 liters or <50% predicted.
C. Peak Expiratory Flow Rate (PEFR) below 200 L/min.
D. Diffusing capacity of the lung for carbon monoxide (DLCO) less than 60% predicted.
E. Residual Volume (RV) to Total Lung Capacity (TLC) ratio greater than 40%.
Question 2
A 62-year-old woman is diagnosed with a 6-cm midline squamous cell carcinoma of the vulva. Because a primary radical resection would require a permanent colostomy, the tumor board recommends treating the vulvar tumour with primary chemoradiation to facilitate sphincter preservation. Pre-treatment 18F-FDG PET/CT shows avid uptake in the right groin lymph node; the left groin is clinically and radiographically negative. The patient is medically fit for surgery and agrees to any indicated nodal procedure before starting chemoradiation. Which groin-node strategy offers the highest chance of regional control with acceptable morbidity?
A. Bilateral sentinel-lymph-node dissection only, then chemoradiation
B. Right inguinofemoral dissection with left sentinel dissection, then chemoradiation
C. Bilateral complete inguinofemoral lymph-node dissections, followed by chemoradiation
D. Definitive chemoradiation to vulva and bilateral groins without nodal surgery
E. Right-groin radiation boost to 60 Gy without nodal surgery; observe the left groin
Answer(s)
Pulmonary Function Testing
Answer 1: B
Explanation:
While multiple parameters from pulmonary function tests (PFTs) can indicate risk, a significantly reduced Forced Expiratory Volume in 1 second (FEV1) is one of the strongest predictors of postoperative pulmonary complications, particularly after major abdominal or thoracic surgery.
Values less than 1.0-1.5 liters or less than 50% of predicted are often cited as indicating high risk. In the prospective, single-centre PREDICT study, 320 adults with known or suspected COPD who were scheduled for major non-cardiac surgery underwent routine spirometry in addition to a standard pre-operative assessment. In multivariable modelling, the only spirometric variable retained was %-predicted FEV₁, which remained an independent risk factor.
According to the PREDICT study, full PFTs add cost and inconvenience without any benefit.
A low FVC (A) also indicates restrictive or obstructive defects, but FEV1 is often more emphasized for postoperative risk. PEFR (C) measures large airway function. DLCO (D) reflects gas exchange capacity and serves as a predictor, but FEV1 often stands out as a more reliable predictor of overall pulmonary complications related to airway clearance and ventilatory capacity. An increased RV/TLC ratio (E) indicates air trapping, which is common in COPD; however, FEV1 is a more direct measure of expiratory airflow limitation relevant to postoperative events.
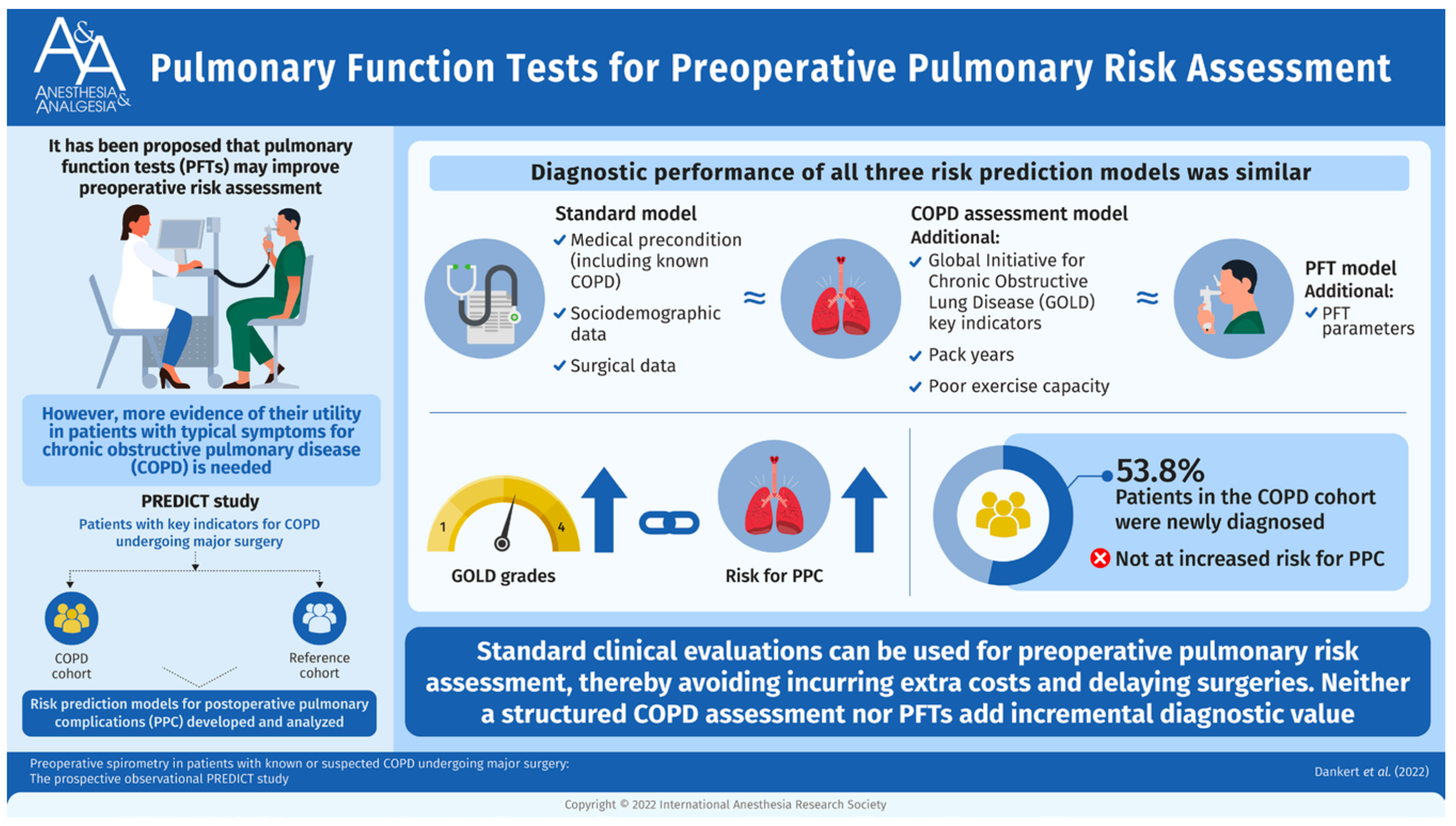
A “full” pulmonary-function test (PFT) panel typically includes all of the following individual tests:
- Baseline (pre-bronchodilator) spirometry
- Post-bronchodilator reversibility spirometry
- Lung-volume measurement (body plethysmography or helium/nitrogen wash-out)
- Diffusing-capacity test for carbon monoxide (DLCO/TLCO)
- Airway resistance / specific airway conductance (Raw, sGaw)
- Maximal voluntary ventilation (MVV)
- Respiratory-muscle pressures – maximal inspiratory & expiratory pressures (MIP/MEP)
- Fractional exhaled nitric oxide (FeNO) – airway-inflammation marker
- Bronchial provocation/challenge test (e.g., methacholine, mannitol or exercise)
- Resting or post-exercise arterial (or arterialised capillary) blood-gas analysis / pulse-oximetry
However, according to the PREDICT study, only SPIROMETRY is predictive of postoperative pulmonary complications. Therefore, in these patients, there is no need to order the FULL PFT; only order spirometry.
Vulvar Cancer
Management Algorithm for Groin-Node–Positive Vulvar Cancer
1. Clinically Negative or PET-Negative Groins (cN0)
| Step | Rationale | Recommended Action |
|---|---|---|
| Groin staging at surgery | Accurate nodal assessment while sparing morbidity | Sentinel-lymph-node dissection (SLND) during vulvar resection for primaries ≤ 4 cm |
| Micro- vs. macro-metastasis | Based on GROINS-V II Risk-adapted therapy limits overtreatment | Micrometastasis ≤ 2 mm: adjuvant inguino-femoral RT (~50 Gy) Macrometastasis > 2 mm or extracapsular spread: completion inguino-femoral lymph-node dissection (ILND) plus groin/pelvic RT ± weekly cisplatin when ≥ 2 positive nodes |
2. PET-Avid or Clinically Enlarged/Fixed Groins (cN+)
| Scenario | Preferred Strategy | Key Points |
|---|---|---|
| Fixed or ulcerated nodes | Definitive chemoradiation (CRT) | Surgery not feasible; aim for ≥ 60 Gy to nodal volume using IMRT/VMAT |
| Resectable PET-avid nodes | Groin dissection followed by CRT | Yields superior overall and locoregional survival versus CRT alone; debulks hypoxic tissue and allows safer RT dosing (based on this publication) |
| Non-operative candidates | Dose-escalated CRT | Escalating groin dose to 59–64 Gy reduces relapse with acceptable toxicity; weekly cisplatin enhances radiosensitivity |
Important Considerations
- Bilateral treatment: cover both groins unless the primary is clearly lateralised and the contralateral SLN is negative.
- Pelvic RT trigger: initiate pelvic fields when ≥ 2 inguinal nodes are positive.
- Manage Toxicity: early physiotherapy, compression garments, and meticulous RT planning limit lymphedema; grade ≥ 3 late effects remain uncommon.
Answer 2: C
If this patient were medically inoperable, the chemoradiation to the groin is an acceptable alternative, but it has a lower 5-year survival. Here is a table of all the studies focusing specifically on the groins:
Radiation dose-response evidence for node-positive groins in vulvar cancer
| # | Study (year) | Treatment setting / cohort | Dose to gross groin nodes† | Key disease-control outcomes |
|---|---|---|---|---|
| 1 | O’Shea et al, 2025 | 88 node-positive pts – surgery + PORT vs definitive CRT | 54 Gy (median) adjuvant; 54–60 Gy definitive | 5-yr locoregional control 69 % (adjuvant) vs 53 % (definitive); 5-yr OS 62 % vs 50 %. Groin relapse 27 % at 54 Gy vs 8 % at 59.4–60 Gy |
| 2 | Richman et al, 2020 | Dose-escalated IMRT, locally advanced | 66 Gy | 76 % clinical CR, 70 % path CR, 2-yr DFS 81 % |
| 3 | Rishi et al, 2020 | High-dose IMRT, locally advanced | 65.4 Gy | 81 % clinical CR |
| 4 | NRG GOG-279, 2024 | Phase II CRT (cisplatin + gemcitabine) | 64 Gy | 73 % path CR, 70 % 2-yr PFS; grade ≥3 toxicity 85 % |
| 5 | Stecklein et al, 2018 | Definitive RT for gross inguinal nodes | 66 Gy (median) | 3-yr groin recurrence 17.7 % (≈82 % control) |
| 6 | Swift et al, 2024 | Retrospective, unresectable groins | ≥63 Gy | Fewer groin failures; only 12.5 % grade 1-2 dermatitis |
| 7 | GOG-205, 2012 | Pre-op CRT for T3-T4 primaries | 57.6 Gy | 64 % clinical CR, ~50 % path CR |
| 8 | GROINSS-V II, 2021 | SLN-positive ≤4 cm tumors | 50 Gy (micromets) | 2-yr isolated-groin recurrence 1.6 % (≤2 mm mets); macromets (>2 mm) 22 % with RT vs 6.9 % with ILND (no chemo with RT) |
| 9 | GOG-37, long-term FU 2009 | Post-ILND adjuvant RT vs pelvic node dissection | 45–50 Gy | 6-yr cancer-specific survival 51 % RT vs 29 % surgery; OS benefit when ≥2 nodes positive |
†Elective groin/pelvic volumes generally received 45–50 Gy; the table lists the dose prescribed to grossly involved inguinal nodes or sentinel-node basin.
Patterns across studies
- Locoregional control consistently improves once the nodal dose surpasses ~60 Gy, especially with concurrent platinum.
- Surgical debulking followed by 50–55 Gy adjuvant RT still provides the best long-term control when surgery is feasible.
- For micrometastatic disease (≤2 mm), 50 Gy alone achieves >98 % groin control and spares full dissection morbidity.
- Dose-escalated IMRT/VMAT (≥64 Gy) yields ≥70 % pathologic CR but at the cost of higher acute grade 3-4 toxicity; careful patient selection is essential.
One spot (starting Sept 2025) open for GYOEDU Coaching and Mentoring for new faculty and those less than 5 years in practice.
Email: support@gyoedu.org to discuss
That's it for this week. Next week, ASCO 2025 edition!
Follow @gyoedu Follow @uppals