Nasogastric Tubes
Suction
Low Intermittent Suction:
Mechanism: In low intermittent suction, the suction is applied at intervals. The suction is turned on for a period and then turned off, allowing rest periods.
Purpose: It's used to mimic the normal physiological process of gastric emptying. The intermittent nature helps prevent constant negative pressure on the gastric mucosa, potentially reducing the risk of mucosal irritation or damage.
Indications: It may be preferred in cases where gentle and gradual decompression is needed or when there's a risk of mucosal damage due to prolonged suction. OR when a tube without a sump channel is the only NG tube available (in some low-cost settings, that may be the case).
Efficacy: While effective, it might be less efficient in rapidly decompressing the stomach than continuous suction, especially in cases of significant gastric output or obstruction.
Continuous Suction:
Mechanism: Continuous suction involves constant negative pressure being applied to the NG tube, continuously removing gastric contents.
Purpose: This method is more aggressive and is used for more efficient and rapid gastric decompression.
Indications: It's often indicated in cases with high-volume gastric output, like in severe gastrointestinal obstruction, significant bleeding, or when rapid decompression is necessary.
Risks: Continuous suction can be more irritating to the gastric mucosa. There is an increased risk of causing local trauma, erosions, or even bleeding due to the constant negative pressure.
In both methods, the suction level (usually measured in mmHg) is typically kept low to minimize the risk of mucosal damage.
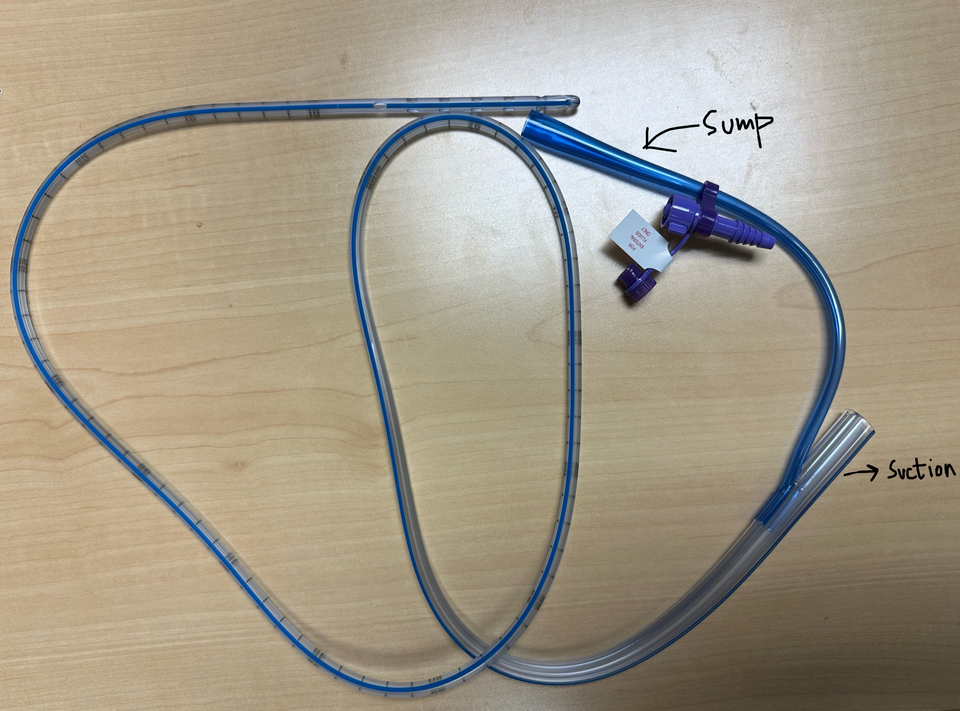
SUMP on NG tube:
In a typical NG tube design, there are two lumens: one for suction and removal of gastric contents and the other (usually blue), which is the sump lumen, for air venting. Here's how the sump works and its purpose:
Air Venting: The sump lumen allows air to enter the stomach, which helps to prevent the suction lumen from adhering to and damaging the gastric mucosa. When suction is applied to the central lumen to remove gastric contents, the sump lumen lets air enter the stomach, equalizing the pressure and preventing the vacuum effect that can cause the tube to stick to and irritate or injure the stomach lining.
Continuous Gastric Decompression: The sump lumen allows for more effective and continuous gastric decompression. It ensures that the central suction lumen remains patent (open and unobstructed) by preventing the formation of a vacuum that can draw the tube walls together, thereby maintaining the tube's functionality for ongoing gastric content removal.
Prevention of Gastric Mucosa Damage: The sump lumen's air vent function reduces this risk significantly by preventing the suction lumen from creating excessive negative pressure that could draw the stomach wall into the tube openings.
Measurement and Medication Administration: In some clinical settings, the sump lumen can also be used for other purposes, such as administering medications or measuring residual gastric fluid volumes, although its primary function is air venting to protect the stomach lining.
Electrolyte Abnormalities
A physiological explanation of the electrolyte abnormalities associated with NG tube use:
Metabolic Alkalosis: The primary mechanism here is the loss of hydrogen ions through gastric suctioning. The stomach secretes gastric acid, primarily hydrochloric acid (HCl), rich in hydrogen ions (H+). When continuously removed, it creates a relative base excess in the body. The kidneys try to compensate by increasing bicarbonate reabsorption and hydrogen ion secretion, but this process is limited. In addition, volume depletion from fluid loss stimulates aldosterone, which enhances potassium and hydrogen ion excretion in the urine, further perpetuating alkalosis.
Hypokalemia: This is multifactorial. Firstly, ongoing losses of gastric fluid rich in potassium lead to direct potassium depletion. Secondly, the body's response to alkalosis includes increased renal excretion of potassium. To help restore the acid-base balance, hydrogen ions (H+) move from the intracellular to the extracellular space. To maintain electrical neutrality, potassium (K+) moves from the extracellular space into cells in the opposite direction. This shift reduces the potassium concentration in the bloodstream, contributing to hypokalemia. Lastly, aldosterone stimulated by volume contraction also promotes renal potassium wasting.
Hyponatremia: This typically results from a combination of factors, including fluid losses from the NG tube leading to volume depletion, which in turn stimulates ADH secretion and water reabsorption, diluting the sodium. Additionally, the loss of sodium in the gastric contents contributes to the deficit.
Hypochloremia: Chloride is a major anion in gastric secretions. Prolonged gastric suctioning leads to significant chloride loss. Chloride loss exacerbates the metabolic alkalosis, as bicarbonate reabsorption is often increased to maintain anion balance.
Low PANiC
Low Potassium (Hypokalemia)
Low Acid (Metabolic Alkalosis)
Low Na (Hyponatremia)
Low Chloride (Hypochloremic metabolic alkalosis)
Insertion
Here is a great video to watch.
When George talks about the valve on the blue end of the sump (@ 3 min 33 sec); this valve is often a big nuisance. When the valve gets blocked, the sump does not let the air into the stomach and the NG tube does not work properly. Always check the valve if patient is not clinically improved but NG tube output is down.
How do you decide it’s time for the NG tube to come out?
Please write your institutional norms on how you decide to remove NG tubes in the comments section.
Follow @uppals